The Baker Act
QUESTIONS AND ANSWERS: BAKER ACT RIGHTS
When a person is taken into custody under the mental health law in Florida and sent for an involuntary psychiatric examination it can be very scary for them and their friends and family. Commonly referred to as a “Baker Act” the initiation of an involuntary exam, what...

The Hidden Dangers of the Baker Act: How Florida’s Mental Health Law is Failing Families
For thousands of Florida parents, the Baker Act has become a nightmare rather than a safeguard. Originally designed as an emergency intervention for those who pose an immediate danger to themselves or others, the law is now widely misused and abused, particularly...

Baker Act? Protect Your Children with 5 Simple Steps!
In 2021, the passage of the School Safety Bill, amended Florida law to require parental/guardian notification prior to the initiation of a Baker Act on a minor child. The intention behind these revisions was to reduce the number of inappropriate Baker Acts on children...

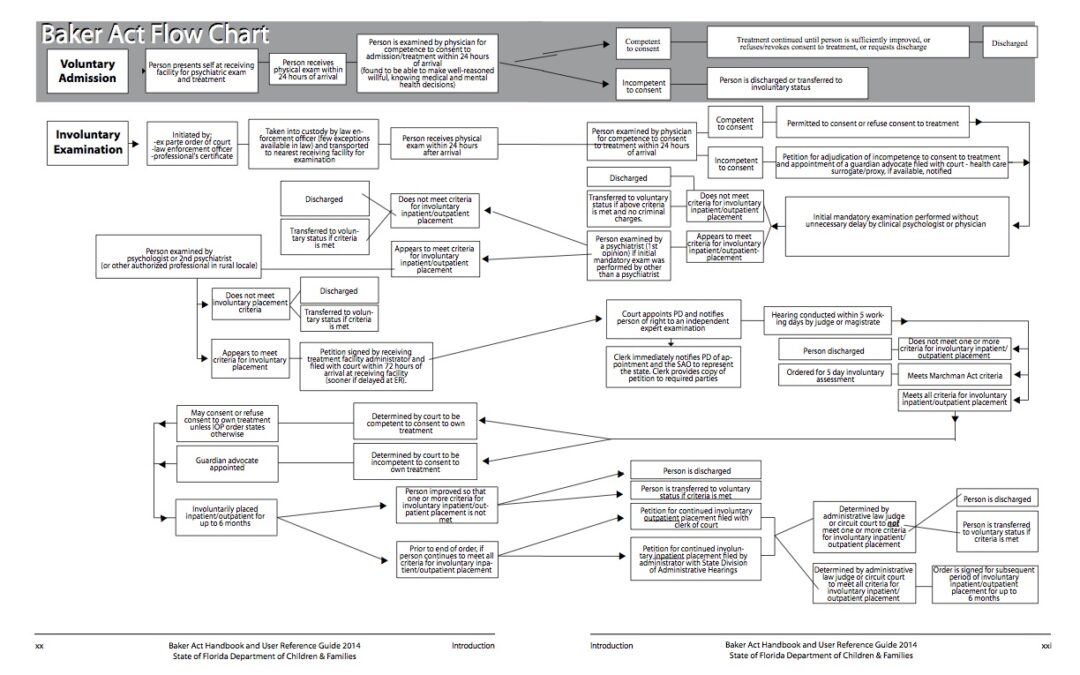
Involuntary Commitment Criteria
The Department of Children and Families, in the state of Florida, lists the criteria for someone to be involuntarily committed. In Florida, this criteria is part of a statute that was passed into law by legislator, Maxine Baker. It is therefore, referred to as the...
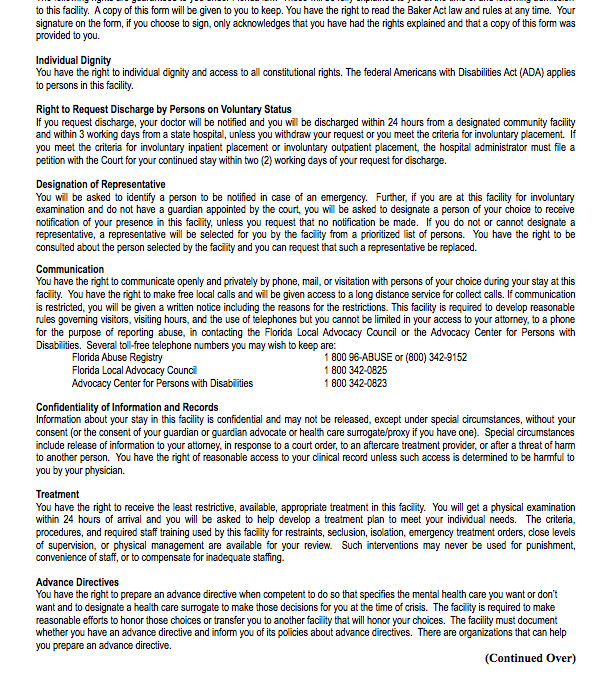
Involuntary Commitment – (Florida Baker Act) — Rights of Individuals
One of the most difficult things regarding involuntary commitment, is understanding what rights the patient, and his or her family members have. Most people find it very difficult to sort through the very complex language of the involuntary commitment law. In the...
Florida Non-Consent Forms
IMPORTANT! Per the Florida statute on involuntary commitment, the school personnel or sheriff resource officer has the legal right to remove your child from school grounds, without your permission, if they feel your child meets the criteria for involuntary commitment....
Involuntary Examination of Minors
It is important for parents to know and understand the mental health law in Florida as this law allows a child to be removed from school and sent for involuntary psychiatric examination without parental knowledge. In order for any person, no matter their age, to be...

Involuntary Commitment Law in Florida
https://www.youtube.com/watch?v=K9kbLhk-0sk Mental Health Involuntary Commitment In Florida, the Involuntary Commitment law is referred to as the Baker Act. If someone you know has been involuntarily committed, you have the right to be fully informed about the...

The Baker Act—Addressing Fraudulent Involuntary Commitment
When authoring the administrative rules for the Baker Act, the Department of Children and Families omitted a rule that would assist authorities in understanding the criteria for invoking state authority to force psychiatric examination. Despite writing numerous other...

Baker Act – FREE HELP & INFORMATION CALL 800-782-2878
What are the time boundaries for the person who has been sent for an involuntary psychiatric examination? Commonly called a Baker Act, involuntary psychiatric examination is a topic that is often misunderstood and misapplied – even by those professionals who are...

